When we hear the word arthritis, we often think of joint pain and stiffness. But did you know that rheumatoid arthritis (RA) can also affect your eyes? Yes, it’s true—RA is not just a joint problem. It’s an autoimmune condition that can cause inflammation in other parts of the body too, including your eyes.
In this blog, we’ll talk about how arthritis can lead to common eye problems, what signs you should watch for, and most importantly, what you can do to protect your eyes and your vision while living with arthritis.
Contents
- 1 What is Rheumatoid Arthritis and How Does It Impact the Body?
- 2 Common Eye Problems Caused by Rheumatoid Arthritis
- 3 What Are the Symptoms of Arthritis in the Eyes?
- 4 Can Arthritis Cause Dry Eyes?
- 5 Scleritis and Episcleritis: Inflammation of the Eye
- 6 Risk of Cataracts and Other Vision Problems in RA Patients
- 7 How Rheumatoid Arthritis Can Increase the Risk of Uveitis
- 8 How to Prevent or Manage Eye Problems Caused by Rheumatoid Arthritis
- 9 Final Thoughts: Don’t Ignore What Your Joints or Eyes Are Telling You
What is Rheumatoid Arthritis and How Does It Impact the Body?
Rheumatoid arthritis (RA) is not just a joint disease—it’s an autoimmune condition, which means your own immune system mistakenly attacks healthy tissues in the body. While most people connect RA with joint pain, swelling, and stiffness, the truth is that this condition can affect many other parts of the body.
Since RA causes inflammation, it can impact organs and tissues beyond the joints—like the lungs, heart, skin, and even the eyes. The inflammation mainly targets connective tissue, and our eyes are full of it. That’s why people with RA often experience eye-related symptoms such as dryness, irritation, redness, and in more serious cases, pain or vision changes.
So, even though RA starts with joint issues, its effects are body-wide. Understanding this connection is the first step toward spotting early signs and protecting your health—including your eye health.
Common Eye Problems Caused by Rheumatoid Arthritis
People with rheumatoid arthritis may experience several eye-related issues due to ongoing inflammation. Here are some of the most commonly linked problems:
- Dry Eyes
- Scleritis
- Episcleritis
- Uveitis
- Peripheral Ulcerative Keratitis (PUK)
- Cataracts and Glaucoma (linked to long-term steroid use)
These conditions can range from mild irritation to serious vision threats. In the next sections, we’ll break down what each of these means and how they affect your eyes.
What Are the Symptoms of Arthritis in the Eyes?
 Rheumatoid arthritis can cause various eye-related symptoms, some of which may appear mild but can indicate underlying inflammation. Watch out for:
Rheumatoid arthritis can cause various eye-related symptoms, some of which may appear mild but can indicate underlying inflammation. Watch out for:
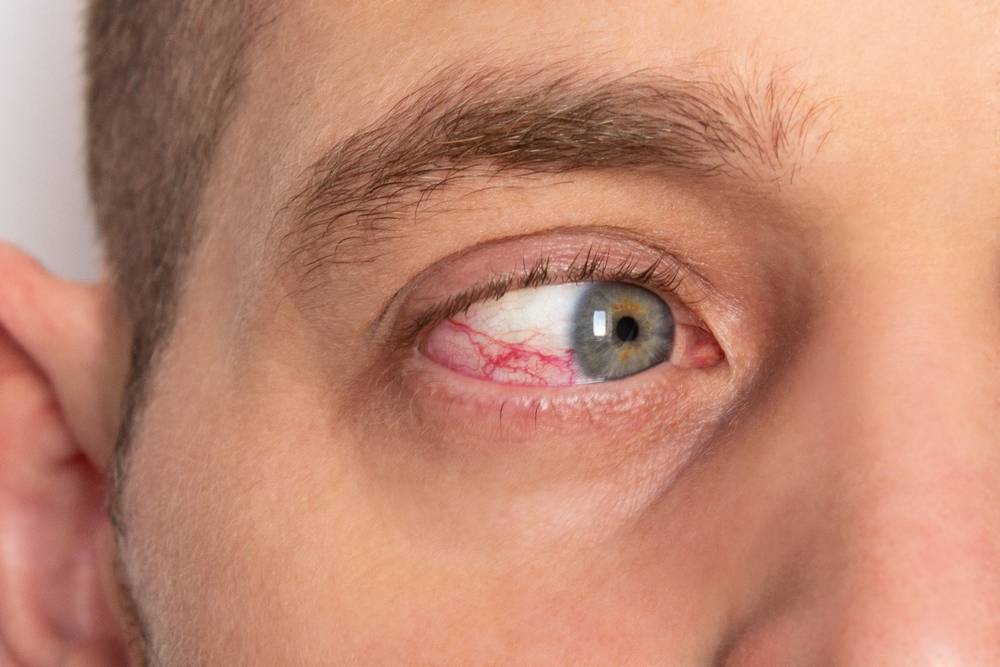
- Eye redness
- Dryness or gritty feeling
- Pain or discomfort
- Blurred or cloudy vision
- Sensitivity to light
- Excessive tearing or watery eyes
- Eye fatigue or pressure
If you notice any of these signs—especially if they are new or persistent—it’s important to consult an eye specialist promptly.
Can Arthritis Cause Dry Eyes?
Yes, rheumatoid arthritis (RA) can definitely cause dry eyes. In fact, dry eyes are one of the most common eye-related symptoms in RA patients. This happens because RA, being an autoimmune disorder, can cause inflammation in the tear glands, especially the lacrimal glands responsible for producing tears.
This condition is known as keratoconjunctivitis sicca—a part of secondary Sjögren’s syndrome, which often occurs alongside RA. When the tear production is disrupted, your eyes may feel:
- Gritty or sandy
- Irritated or itchy
- Red and inflamed
- Sensitive to light
- Tired, especially after reading or screen time
If left untreated, dry eyes can lead to more serious complications like corneal damage or infection. That’s why managing dryness early with artificial tears, lubricating gels, or medications is crucial for people living with RA.
Scleritis and Episcleritis: Inflammation of the Eye
 In some cases, rheumatoid arthritis doesn’t just stop at dry eyes — it can lead to more serious inflammation in different layers of the eye, namely scleritis and episcleritis.
In some cases, rheumatoid arthritis doesn’t just stop at dry eyes — it can lead to more serious inflammation in different layers of the eye, namely scleritis and episcleritis.
-
Episcleritis is a milder form. It affects the thin layer of tissue covering the white part of the eye (sclera). It usually causes redness, mild pain, and irritation, and often gets better with minimal treatment.
-
Scleritis, on the other hand, is more severe. It involves deeper inflammation in the white part of the eye and can be quite painful. People with scleritis may experience:
- Deep, intense eye pain
- Redness and swelling
- Blurry vision
- Sensitivity to light
Scleritis can even lead to vision loss if left untreated. Sinc e this type of inflammation is directly linked to RA’s autoimmune response, prompt diagnosis and treatment from a rheumatologist and eye specialist is essential.
Risk of Cataracts and Other Vision Problems in RA Patients
People with rheumatoid arthritis face a higher risk of developing eye problems beyond just inflammation. One of the most common concerns is cataracts — a clouding of the eye’s natural lens that can blur vision and affect daily life.
Here’s why RA patients are more at risk:
- Corticosteroid medications, often prescribed to manage RA inflammation, can lead to cataract development when used over long periods.
- Chronic inflammation in the body, including around the eyes, may contribute to other vision issues such as glaucoma (increased pressure in the eye) or macular edema (swelling in the central retina).
These conditions don’t always show early symptoms, which is why regular eye check-ups are crucial for anyone managing RA. Early detection can help prevent long-term damage and preserve vision.
How Rheumatoid Arthritis Can Increase the Risk of Uveitis
Uveitis is a condition where the middle layer of the eye (called the uvea) becomes inflamed. While it can happen for many reasons, autoimmune conditions like rheumatoid arthritis (RA) are known triggers.
In RA, the body’s immune system mistakenly attacks its own tissues — and sometimes, it targets the eye. This immune response can lead to inflammation in the uvea, causing pain, redness, blurred vision, and sensitivity to light.
If left untreated, uveitis can lead to serious complications like:
- Permanent vision loss
- Retinal damage
- Glaucoma or cataracts
Because uveitis can worsen quickly, it’s important for RA patients to report any changes in vision or eye discomfort to their doctor immediately. Early treatment — often with anti-inflammatory eye drops or immunosuppressants — can help protect vision and manage the inflammation effectively.
How to Prevent or Manage Eye Problems Caused by Rheumatoid Arthritis

Living with Rheumatoid Arthritis doesn’t just mean joint pain — it can also affect your eyes. But with a few mindful habits, you can manage both RA and eye health together. Here’s how:
- Don’t skip your regular eye check-ups: Just like your joints, your eyes need routine attention — especially if you’re living with RA.
- Be alert to changes: Redness, blurry vision, dryness, or eye pain can be early signs of RA-related eye problems. The sooner you act, the better.
- Stick to your RA treatment plan: Keeping inflammation under control through your medications helps reduce its effects on your eyes too.
- Use prescribed eye drops for dryness: If you experience dry eyes, lubricating eye drops or medicated options can bring relief and prevent complications.
- Discuss steroid use with your doctor: Long-term steroids, often used in RA, may increase your risk for cataracts. Ask your doctor about safer alternatives if needed.
- Protect your eyes from dryness and dust: Wear sunglasses when outdoors and use humidifiers indoors, especially in dry or air-conditioned environments.
- Eat a balanced, eye-and-joint-friendly diet: Foods rich in omega-3 (like flaxseeds, walnuts, fish), antioxidants, and vitamin A support both joint and eye health.
- Stay hydrated: Water helps maintain joint flexibility and also keeps your eyes moist and comfortable.
👉 Whether it’s your joints or your vision, timely care and regular monitoring can make a huge difference. If you’re facing eye symptoms or joint issues, don’t wait — consult a specialist today to protect your long-term health.
Final Thoughts: Don’t Ignore What Your Joints or Eyes Are Telling You
Rheumatoid Arthritis doesn’t just stop at the joints — it can slowly impact your eyes and overall quality of life if not managed well. Whether it’s persistent joint stiffness or sudden eye discomfort, listening to your body is key.
🩺 Need expert help for joint pain or RA?
Talk to an experienced online orthopedician on MantraDoc and get personalized guidance from the comfort of your home.
Facing eye issues like dryness, redness, blurry vision, or even early cataracts? Don’t wait for it to worsen.
👉 Book your free appointment with the experts at Eye Mantra – India’s leading eye hospital, or call us at +91 9711116605 for instant support.